I’ve recently finished a 3.5-hour exclusive video series for my clients outlining the latest research on supplements and herbs in Inflammatory Bowel Disease for the IBDCoach program. To my knowledge, it’s the most compressive and accessible overview of this specific subject ever created.
In recent years, one herb that has received the lion’s share of attention has been used since roughly 3500 BCE by Proto-Indo-Europeans in a ceremonial context. Over the last 3 decades, it has arguably revealed more about human biology than any other plant. It’s time to talk about the promise and pitfalls of cannabis and its truly extraordinary interactions with the body, gut, and brain.
Examining the Evidence of Cannabis in IBD
Compared to other herbs, there has been a moderate amount of science directly related to cannabis and Inflammatory Bowel Disease. One thing is for sure: a notable portion of IBD patients use cannabis, anywhere from 10% to 50%.1
IBD animal studies with cannabis have demonstrated promising results but few human studies and controlled trials have been conducted. In a recent review paper, researchers determined that the data was mixed. Of 5 academic publications, only 2 demonstrated a positive correlation in disease activity, while the remaining 3 showed little to no benefit in the probability of achieving remission.2 Evidence does suggest that IBD patients’ quality of life improved with cannabis use in addition to other secondary symptoms of IBD like the quality of sleep and significant increases in appetite. In 4 survey studies with 273 UC and 595 CD patients conducted between 2013 – 2017, the majority of patients reported significant reductions in pain and nausea and improvements in appetite.
Dr. Christian Turbide at a Crohn’s Disease and Ulcerative Colitis Canada Conference reported on a nationwide inpatient survey of patients with IBDrevealed some pretty interesting results including lower rates of colectomy and mortality when comparing cannabis users to non-cannabis users.3 This study correlating reports of marijuana usage and IBD outcomes, however, cannot uncover a causal relationship between these two factors. There is a clear need for randomized, controlled studies on the impacts of cannabis on IBD symptoms and secondary effects of IBD to better confirm the link between cannabis and IBD. The underlying mechanisms of cannabis activity in the brain and body may provide some insight into how this plant may benefit people with Crohn’s disease, ulcerative colitis, or microscopic colitis.
Interested in Other Emerging Therapies for IBD? Read About Psychedelics and IBD
Cannabis and Human Biology:
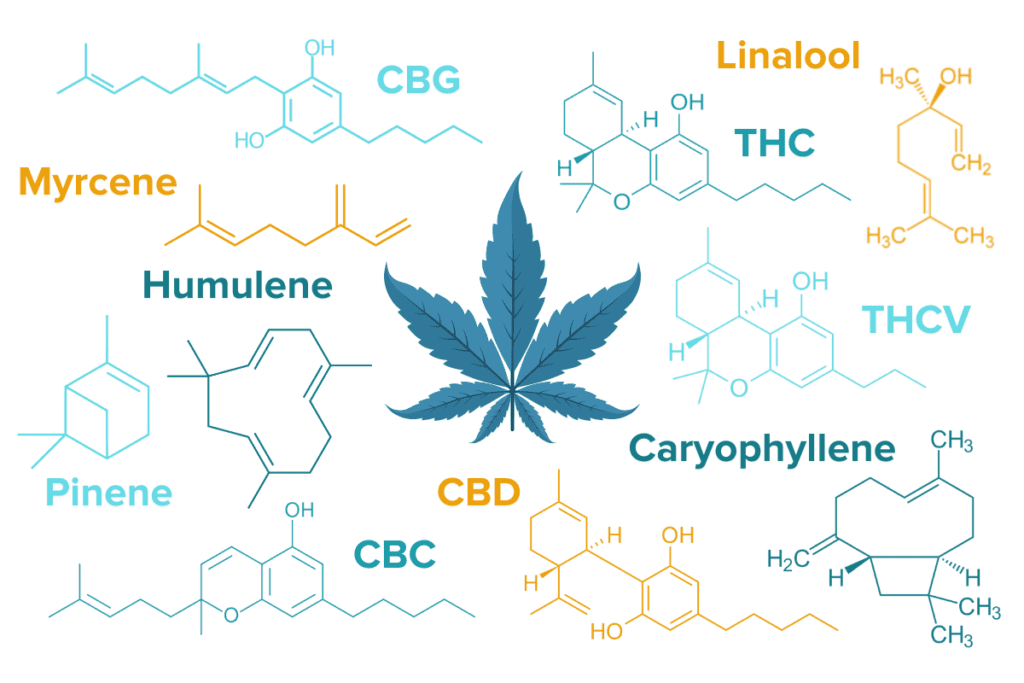
The cannabis plant itself is extraordinarily complex. It contains over 483 classes of molecules, many of which are believed to have a biological effect in mammals. Two of the main compounds are called cannabinoids and terpenes. Cannabinoids include THC, CBD, THCV, CBC, CBG, CBN, and nearly 100 others, and though THC and CBD are best-known, several more have also demonstrated therapeutic potential, especially in modulating inflammation.4 Over 120 known terpenes such as Myrcene, Caryophyllene, Linalool, Pinene, Humulene, and Limonene are responsible for the floral and aromatic qualities of marijuana flowers. 5
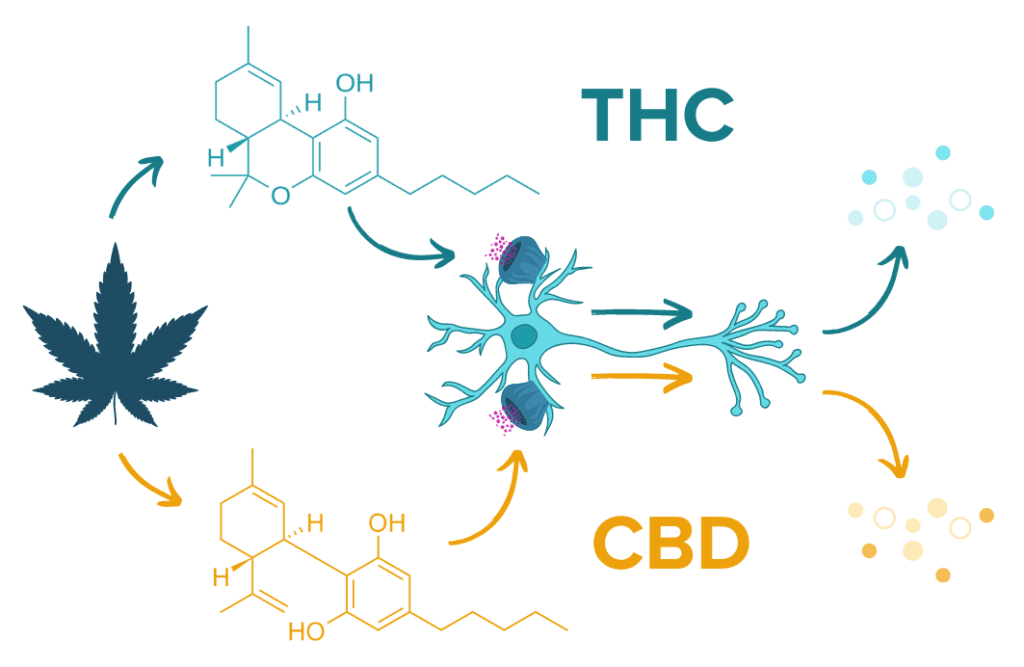
The endocannabinoid system, only discovered in the early 1990s, is a widespread receptor system throughout the body and is involved with more functions than we could review: inflammation, appetite, mood, pain, cognition, nausea, vomiting, and multiple interactions in the GI system among others. The endocannabinoid system can respond to both endogenous cannabinoids (cannabinoids produced by our own body) and exogenous cannabinoids like those introduced to the body from cannabis plants. The two primary endogenous endocannabinoid neurotransmitters, anandamide and 2-AG,6 may even help modulate the microbiome6 and the gut-brain axis.7
There are two main cannabinoid receptor types: CB1 and CB2. The CB1 receptor is primarily located in the central nervous system and affects memory processing, motor regulation, appetite, pain sensation, mood, and sleep. CB2 is primarily found in the peripheral nervous system and is involved in the immune response. Multiple in-vitro studies (meaning studies conducted in the lab with methods like cell culture samples) demonstrated that CB1 and CB2 receptor agonists (activating agents) ameliorated GI inflammation in murine (mouse) models while CB1 and CB2 antagonists (deactivators of the CB1 and CB2 receptors) had the inverse effect.2
Strain Matters with Cannabis and IBD
Though we often discuss the Cannabis sativa plant as if it were a monolith, this one species can express an enormous range of combinations of cannabinoids and terpenes from one strain to the next. Each unique chemical composition can produce a distinct collection of psychotropic and biological responses. For example, CBD-dominant strains have risen in popularity due to CBD’s anti-inflammatory properties and reduced psychoactive effect. This is fueled by the unique interaction between cannabinoids and their receptors in the human body. CBD binds to the CB1 rector and causes an inverse chemical cascade compared to that produced when THC binds to the CB1 receptor.8 Terpenes are also responsible for different biological effects and vary in their ability to attenuate inflammation, reduce anxiety, or demonstrate anti-microbial activities.5
Scientific research has not yet had the chance to extensively compare the effects of specific strains of Cannabis sativa, but this research could help determine which cannabinoid and terpene profiles are most appropriate and efficacious in addressing disease mechanisms. One stumbling block is that the United States federal government still classifies cannabis as a Schedule I controlled substance.9 (Schedule I is reserved for substances with the highest potential for abuse and no medical benefit. By comparison, methamphetamine and oxycodone are classified as Schedule II, which recognizes the medical benefits and allows the substances to be prescribed by physicians.) Additionally, the cannabis material made available for scientific research in the US is solely supplied by the National Institute of Drug Abuse (NIDA) from one single crop grown at the University of Mississippi.10 This means that even when studies on the effects of cannabis are approved, researchers only have access to a mere fraction of the genetic diversity the plant is capable of, so studies of strain comparison are impossible.
Despite these barriers to research on the potential benefits of cannabis use for conditions like IBD, there is a growing wealth of case reports and anecdotal evidence to support the use of cannabis for these chronic conditions. Many people with IBD who live in states that have approved medicinal or recreational marijuana have added to this growing body of evidence. Looking forward, the growing acceptance of cannabis in the US has the potential to fuel more research incentives and improve researchers’ access to diverse cannabis strains.
Read More About Other Emerging Treatments for IBD
My Personal Experience with Cannabis in Crohn’s Disease
My personal experience with cannabis has been overwhelmingly positive, especially when I am flaring. I can reliably turn to a mixture of CBD and THC to address symptoms that defy all my other interventions. A Crohn’s flare brings feelings of tightness, muscle spasms, and pain in my lower right abdominal quadrant, and vaping or smoking a small amount of a CBD/THC blend almost instantly takes the tightness away in the moment. I am grateful to have access to cannabis for in-the-moment relief for acute pain symptoms, but I do, however, feel that other interventions such as diet, other herbs and supplements, and even lower-end medications may have longer-lasting and more robust effects on inflammation. And while I do experience side effects from prolonged cannabis use in the form of feeling “washed out” the next day (with reduced memory and motivation), I also find it can improve my creativity and overall wellbeing.
Working with Your Medical Team on If and How You Can Incorporate Cannabis into Your IBD Protocol
If you do decide to explore cannabis for relief with a chronic medical condition, I have some tips:
- Be open and honest with your GI and other health team members about your cannabis use. If you feel judged, dismissed, or not listened to, this could be an indication to work on refining your health team.
- Consider reaching out to a cannabis specialist who not only has experience in just “recommending” cannabis generally, but will instead offer guidance on usage and strain. (Access to these specialists can vary widely by geography, so please ask in our community for help if needed.).
- Always comply with your local state or country laws around cannabis. If, cannabis is inaccessible to you, remember that no single variable discussed in the IBDCoach program will “make” or ”break” your IBD protocol.
- Obtain laboratory data on any cannabis product you buy to understand the cannabinoid or/and terpene concentrations. You will undoubtedly find some strains that work better for you than others and are suited for different purposes, and the lab data can help you with your future product selection. For example, many individuals find they prefer Indica strains (higher in CBD) at night and Sativa strains (higher in THC) during the day. If the next time you shop you cannot find the specific strain that helped the most, you will have the lab data on hand and can find something with a similar chemical profile.
- Start slow and monitor side effects and possible interactions. Make sure you are staying motivated, happy, and keeping up with work. Sometimes with cannabis, less is more. A small amount can often go a long way and having more may not improve your outcome.
- Lastly, understand that this is a mysterious and under-researched tool with a complex composition. Pay attention not only to which strain you consume but also your context of consumption. What setting works best for you? What time of day? What location? What type of mood is most suitable for you to be in to get the most benefit? Which type of IBD symptoms does it work best for and which does it not?
In conclusion and as echoed in almost every study, review paper, and meta-analysis on the subject: more research is needed to understand the full impact of cannabis on IBD symptoms and outcomes. In the future, researchers may consider joining forces with advanced cannabis growers to develop strains specifically targeted for IBD in their cannabinoid and terpene profiles. Hopefully, as a more sensible drug policy is enacted in the United States and around the world, the specific medicinal benefits or lack thereof will be elucidated in IBD.
- Scott FI. Marijuana Use in Inflammatory Bowel Disease: Understanding the Prevalence and the Potential Pitfalls. Crohns Colitis 360. 2020;2(2). doi:10.1093/crocol/otaa016
- Picardo S, Kaplan GG, Sharkey KA, Seow CH. Insights into the role of cannabis in the management of inflammatory bowel disease. Ther Adv Gastroenterol. 2019;12:1756284819870977. doi:10.1177/1756284819870977
- Crohn’s and Colitis Canada. Cannabis and Inflammatory Bowel Disease.; 2019. Accessed April 14, 2021. https://www.youtube.com/watch?v=TIMh2R49HgQ
- Cannabis (Marijuana) and Cannabinoids: What You Need To Know. NCCIH. Accessed February 27, 2022. https://www.nccih.nih.gov/health/cannabis-marijuana-and-cannabinoids-what-you-need-to-know
- Booth JK, Bohlmann J. Terpenes in Cannabis sativa – From plant genome to humans. Plant Sci Int J Exp Plant Biol. 2019;284:67-72. doi:10.1016/j.plantsci.2019.03.022
- Lu HC, Mackie K. An introduction to the endogenous cannabinoid system. Biol Psychiatry. 2016;79(7):516-525. doi:10.1016/j.biopsych.2015.07.028
- Sharkey KA, Wiley JW. The Role of the Endocannabinoid System in the Brain-Gut Axis. Gastroenterology. 2016;151(2):252-266. doi:10.1053/j.gastro.2016.04.015
- Peres FF, Lima AC, Hallak JEC, Crippa JA, Silva RH, Abílio VC. Cannabidiol as a Promising Strategy to Treat and Prevent Movement Disorders? Front Pharmacol. 2018;9:482. doi:10.3389/fphar.2018.00482
- Drug Scheduling. Accessed February 27, 2022. https://www.dea.gov/drug-information/drug-scheduling
- Marijuana Research | Ole Miss. Marijuana Research. Accessed February 27, 2022. https://pharmacy.olemiss.edu/marijuana/





