Living with a chronic gastrointestinal condition like Crohn’s disease or ulcerative colitis affects far more than just your gut health. A personalized treatment plan for IBD isn’t the only essential component for achieving and maintaining remission from IBD. Managing and adapting your treatment plan over time, understanding the long-term risks and complications associated with living with IBD, monitoring disease progression, and navigating the mental and emotional toll of living with IBD are all a part of the journey that is inflammatory bowel disease.
There’s More to IBD
Digestive conditions are on the rise around the world but they are often overlooked and little discussed. Despite there being more than 7 million global cases of IBD,1–3 many people still confuse IBD with similar conditions like IBS or have never even heard of it before. Lesser-known IBDs like collagenous colitis and lymphocytic colitis are rarely discussed despite them potentially becoming even more common than Crohn’s and UC.4–6 Symptoms of IBD and other GI conditions are often considered taboo or too private to freely discuss, so people are left alone to defend against the many struggles of living with this condition. There is so much more to inflammatory bowel disease than many people realize. IBD is a very real and very debilitating condition that impacts millions of people around the globe. It’s time to give IBDers the attention they deserve and to help people with IBD gain freedom from their condition and thrive in remission.
What is IBD?
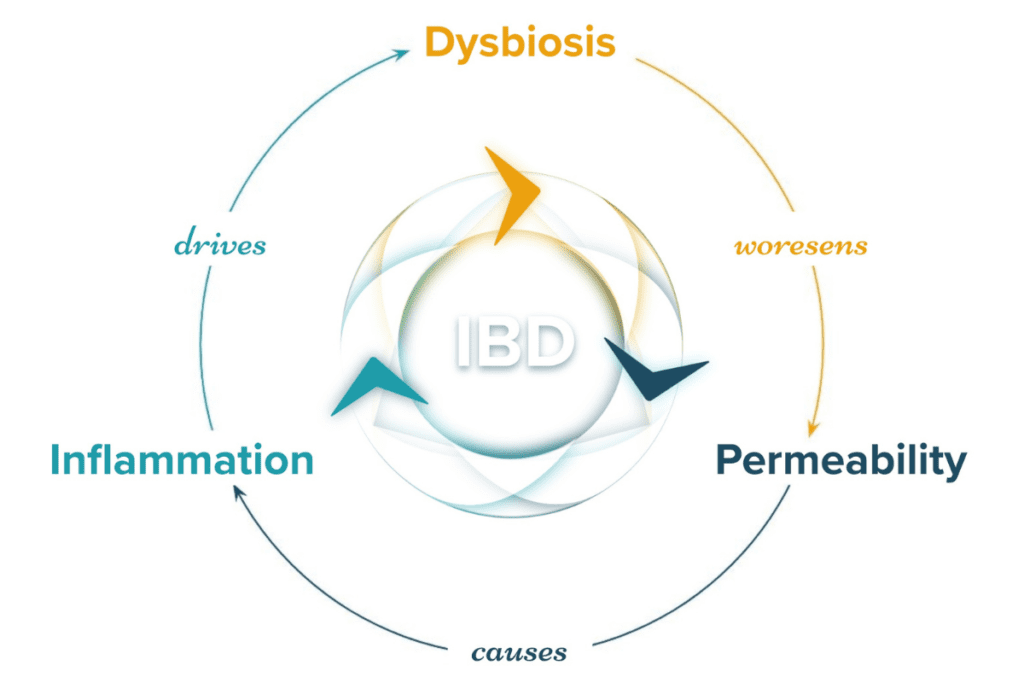
The inflammatory bowel diseases are idiopathic and chronic immune-mediated conditions including Crohn’s disease (CD), ulcerative colitis (UC), and microscopic colitis (MC) that affect all or specific parts of the gastrointestinal tract.7–9 A dysregulated immune response in the mucosal membrane of the GI tract results in inflammation of the tissue and subsequent symptoms and complications.10,11 At this time, there is no clearly defined cause of IBD. Both genetic and environmental factors appear to contribute to the onset of IBD, but every single case’s cluster of risks and causative factors is different.12–19 There is no permanent cure for IBD at this time. Therefore, both therapeutic and lifestyle interventions are often needed for the successful long-term management of this condition.10,20–26
Learn More About the Science Behind IBD in Part One of This Series Here.
Treatments for IBD
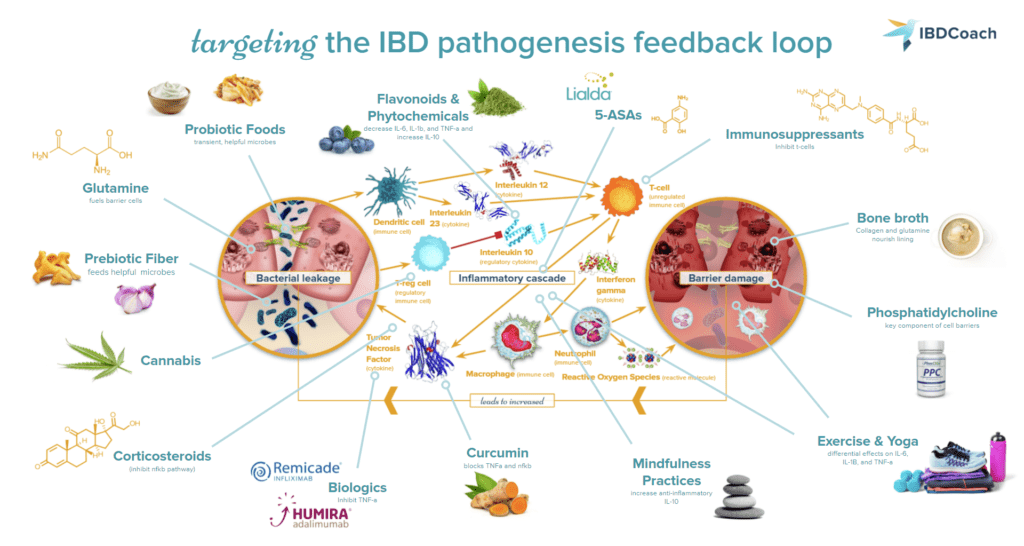
The treatment of inflammatory bowel disease is evolving every single day. No two cases of IBD are alike because IBD occurs on an incredibly diverse spectrum influenced by almost infinite genetic and environmental risk factors. Because of this, there is no singular “best treatment for IBD.” Achieving remission from IBD typically requires a personalized balance of both medical and natural approaches to healing from IBD. Medications, surgical interventions, dietary alterations, lifestyle changes, and more may all play a role in developing the perfect treatment plan for CD, UC, or MC. Investigative treatments such as psychedelic-assisted therapy,27–29 fecal microbial transplants, or hyperbaric oxygen therapy may someday play a role in supporting remission for some IBDers. Each IBDer is their own best judge about what is working well in their treatment plan. Let’s take a closer look at what life with IBD looks like.
Learn More About the Best Treatment Strategies for IBD in Part Two of This Series Here.
The Progression of IBD Over Time
Because IBD is considered a lifelong condition, one thing that most people wonder when they or a loved one are newly diagnosed is, “What will the rest of my life look like with this condition?” A lifetime with IBD looks different for everyone, but there are a few things that every IBDer should be prepared for on their journey, such as how to navigate information about cures for IBD, what to expect from IBD flares, and which complications are commonly related to IBD.
The Cure for IBD
One more time, for the record: at this point, there is no cure for IBD. In technical terms, a cure is considered a permanent resolution of a condition or ailment. Unfortunately, no medication, diet, or lifestyle intervention can permanently resolve inflammatory bowel disease. Many people with IBD often feel that they are “cured” when they enter into a deep state of remission and their symptoms of IBD remain dormant for a long period, but a recurrence of disease activity, known as a flare, is always possible. Understanding this about IBD is essential to ensuring that IBDers can develop a plan to maintain remission for as long as possible but also prepare to address a flare, should one happen, instead of feeling completely blindsided by a sudden onset of IBD symptoms.
IBD Flares
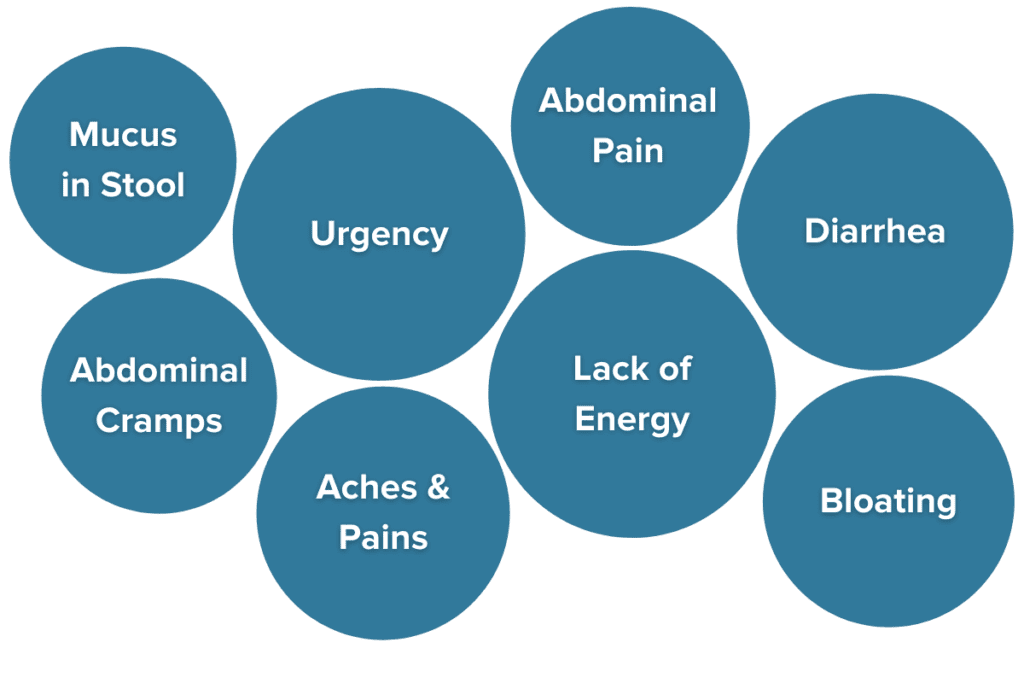
When symptoms of IBD return after a period of remission, it is known as a flare. For many, flares can feel sudden, disheartening, and isolating. Flares can include any of the following symptoms of IBD:
- Frequent and urgent bowel movements (often over ten a day)
- Persistent diarrhea or constipation
- Blood and mucus present in the stool (except in microscopic colitis)
- Painful cramping
- Abdominal pain
- Whole-body aches and pains
- Unintentional weight loss and malnutrition
- Fatigue30,31
In addition to experiencing a recurrence of symptoms of IBD, flares can be emotionally challenging. It can feel nearly impossible to engage in social activities, get out of the house, work a full-time job, and more. Brain fog, feelings of depression, or feeling like a failure for having symptoms come back are commonly reported during flares.
Flares will happen. It isn’t a failure, it is just how IBD works.
The best thing people with IBD can do is to have a plan in place to tackle a flare should one arise to get back into remission as quickly as possible. At IBDCoach, we help our members develop their personalized Remission Master Plans to do exactly that. Changing medication strategies, managing stress, adjusting diet, and more can all play a role in getting back on track when a flare happens.
To learn more about how to build your RMP, attend our FREE Microcourse, the Foundations of Remission, today.
Complications of IBD
Over time, people with IBD may experience or be at risk of experiencing certain complications related to their IBD. Complications are unfavorable results of a condition that can adversely affect life outcomes. Some complications may even be life-threatening.
Common complications of Crohn’s disease include:32
- Strictures: narrowed intestinal passages caused by thickening of the bowel wall and scar tissue. May result in intestinal obstructions. 33
- Intestinal obstruction: the inability of material to pass through the GI tract, known as an obstruction, is one of the most common complications of CD. Signs of obstruction include vomiting and crampy abdominal pain.
- Fistulas: passageways developed from deep ulcers, sores, or abscesses that connect from the GI tract to somewhere else such as the vagina or near the anus. Roughly 20-50% of CD patients develop a fistula.34 If untreated, fistulas can lead to serious infection.
Common complications of ulcerative colitis include:
- Toxic megacolon: dilation and extreme swelling of the colon may result from severe inflammation in UC. If the colon becomes too dilated, it loses its ability to contract which causes a buildup of gas. Toxic megacolon results in extreme acute illness, including GI pain and distension, fever, and tenderness in the abdomen, and immediate medical attention is required.35
- Colorectal cancer: somewhere between 5-8% of patients with UC may go on to develop colon cancer within 20 years of their UC diagnosis.36,37 In CD, the risk is greatest in individuals with colonic disease activity.
Complications are most commonly related to long periods of excessive, uncontrolled disease activity and inflammation.38,39 One of the best ways to defend against complications of IBD is to achieve and maintain remission. If complications should arise, knowing the signs and getting treatment quickly are essential to avoid progression and life-threatening risks.
Understanding Additional Risk Factors
Inflammation and chronic health conditions take a toll on the body and mind. Individuals who suffer from one chronic condition, such as IBD, are substantially more likely to suffer from additional chronic health conditions, especially those relating to immune activity, stress, and inflammation. Most notably, individuals with IBD are more likely than non-IBDers to suffer from certain comorbid conditions (additional diagnoses) and may be at an elevated risk of developing certain forms of cancer.
IBD and Comorbid Conditions
Roughly 78% of IBDers also have a diagnosis of at least one other health condition.40 These comorbid conditions can influence the best treatment options and long-term outcomes of living with IBD. Comorbidities may require additional medications, lifestyle changes, or other dietary changes that must be taken into account with treatments utilized for IBD. While we will not cover all the possible comorbid conditions it is possible to be diagnosed with, some of the most commonly diagnosed comorbid conditions include:
While arthropathies are a common EIM in people with IBD, many IBDers also have a diagnosis of arthritis.41 Unlike arthralgia, where joint aches and pains are not accompanied by inflammation, arthritis presents with inflammation. Certain biologics may have benefits for both arthritis and IBD activity.42
Almost 30% with IBD also suffer from depression or anxiety, a rate almost twice that of the non-IBD population.43–45 Interestingly, certain medications for depression, such as bupropion, may have a positive benefit for symptoms of IBD due to interactions with the gut-brain axis and because of the role that stress may play in exacerbating symptoms of IBD.46,47
One study suggests that up to a third of IBDers experience symptoms of post-traumatic stress disorder (PTSD) following their IBD diagnosis.48 Symptoms of PTSD can include hypervigilance, intrusive memories, nightmares, negative changes in thinking and mood, and more, and may dramatically impact an individual’s normal daily functioning and quality of life. Stress is heavily associated with disease activity and flares in IBD, so successfully managing symptoms of PTSD and other stress-related conditions can improve the chances of achieving and maintaining remission.49–52
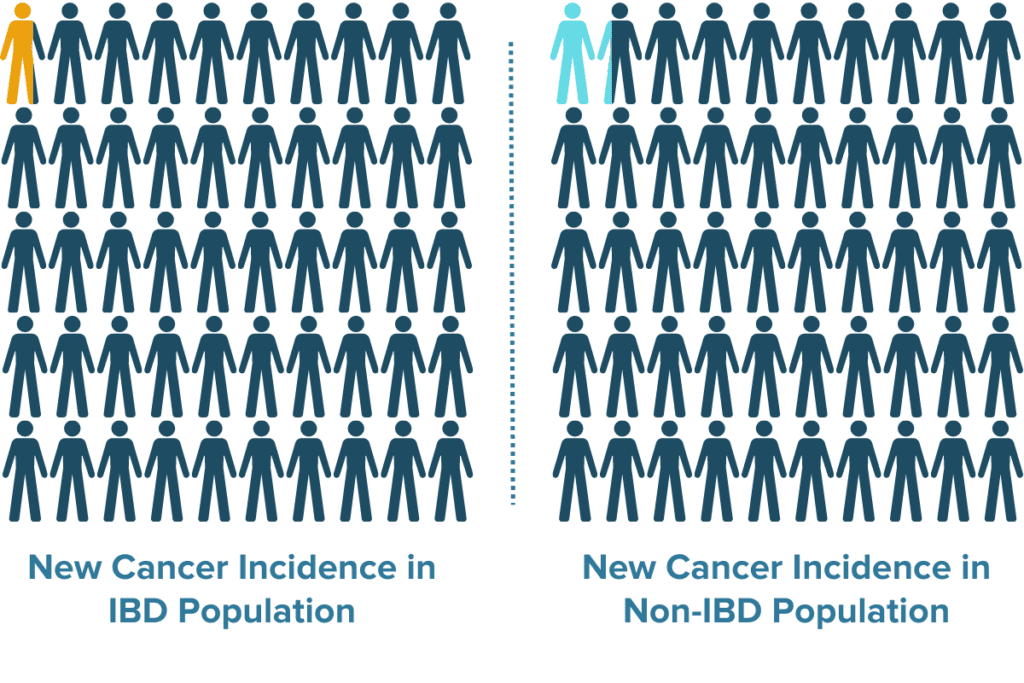
IBDers may be at increased risk for developing certain cancers, especially colorectal cancer.36 The risk of developing cancer in people with IBD is increased by disease severity, prolonged intestinal inflammation, and increased duration of active/uncontrolled disease.38,39 Certain medications for IBD are also associated with an increased risk of cancer.53,54
Studies have indicated that celiac disease may be a risk factor for IBD and that celiac disease is more common in IBDers than in the general population.55 Having celiac disease in addition to IBD may influence which dietary strategies are most suitable for an individual.
Comorbid conditions can influence the best path forward concerning lifestyle interventions, dietary changes, and treatment strategies that are best suited to address an individual’s IBD and other health concerns. In some cases, treatment options may be synergistic and promote the improvement of both conditions. In other cases, doctors may need to watch out for contraindications or harmful interactions between medications. Either way, understanding the unique history and needs of each individual is the best way to successfully tailor treatment strategies and promote health and wellbeing.
IBD and Cancer Risk
One of the most common concerns for IBD and its treatment options is the understanding that IBD and certain medications for IBD are known to increase cancer risk. Understanding all factors that impact the risk of developing cancer for people with IBD in the context of each unique case can help better inform decision-making and allow IBDers to minimize their cancer risk as much as possible.
Biologics and Cancer Risk
Elevated cancer risk due to the use of biologics and immunosuppressants is one of the most commonly cited reasons that many individuals with IBD wish to pursue an all-natural IBD treatment plan. While it is true that evidence demonstrates biologics and immunosuppressants can make individuals more likely to develop certain forms of cancer including lymphomas and melanomas, the overall risk of developing cancer due to medication use is still low overall.53,56 Additionally, many other studies have concluded that biologic or immunosuppressant monotherapies may not increase overall cancer risk at all or that other factors are important in influencing this risk.53,57 Some biologics may even have anti-cancer benefits (for some forms of cancer) due to their role in certain immune pathways.58 Studies often have short follow-up timelines and have participants with diverse medical histories, diets, or lifestyle protocols that further contribute to differences in overall cancer risk. This has led to an array of mixed evidence and confusion regarding the true cancer risk in patients with IBD.
Before avoiding medications for IBD altogether in an attempt to minimize cancer risk, remember that medications are not the only factor that influences cancer risk, so natural treatments for IBD will not reduce your risk to zero.
Uncontrolled IBD and Cancer Risk
Compared to the general population, one of the greatest cancer threats that people with IBD face is an elevated risk of developing colorectal cancer. Roughly 5-8% of patients with UC will develop colorectal cancer within 20 years of their diagnosis. While UC has a greater risk of colon cancer than CD, cases of CD with high colonic disease activity may also be at an elevated risk for this development. Colorectal cancer risk in IBD patients is influenced most strongly by two key factors:
- Length of time since diagnosis
- Duration of active inflammation and uncontrolled disease activity59
While IBDers cannot control the age at which they were diagnosed, it is well evidenced that having longer periods of high inflammation and disease activity, such as in uncontrolled flares, is one of the strongest predictors of increased colorectal cancer risk. Some sources suggest that the risk of colorectal cancer in individuals with IBD has declined to match the risk observed in the non-IBD population. One reason cited for this decline in cancer risk is that treatments for IBD that control intestinal inflammation have improved substantially in recent history.60 This evidence suggests that one of the best things that people with IBD can do to reduce their risk of developing cancer is to control inflammation and achieve and maintain remission.
Overall, the incidence of new cancer diagnoses of any kind is not different between people with and without IBD, even when medications are considered.61 In some cases, IBDers may opt to avoid medication use in favor of more natural treatments of IBD hoping to avoid the increased risk of cancer, not understanding that taking longer to achieve remission may also increase their cancer risk. One of the most powerful tools for reducing inflammation is the use of IBD medications along with a well-rounded dietary and lifestyle plan.
Managing your IBD Treatment Plan
Because IBD is a lifetime condition, understanding how to manage and IBD your IBD treatment plan over time is an ongoing task for most individuals with IBD. IBD is a multifaceted condition with complicated treatment considerations that vary substantially from person to person. No two treatment plans for IBD will ever look the same, and it is also very likely that one person’s “perfect IBD treatment strategy” may evolve over time or may even evolve day-to-day based on changes in symptoms and circumstances.
To Learn More About Specific Treatments of IBD, Read Part 2 of This Series: Treatments for IBD.
Managing an IBD treatment plan can mean many things: building and adapting your team of healthcare professionals to better suit your unique needs, monitoring your symptoms of IBD to assess treatment progress or watch for signs of a flare, using lab tests of inflammatory marks to help keep a better eye on disease activity, developing a personalized flare protocol, and even changing and adapting your treatment goal over time as your needs, goals, and IBD activity change.
Building a Diverse Medical Team
Overcoming IBD requires a well-rounded treatment approach. While every single case of Crohn’s, UC, and MC is unique, almost everyone requires some combination of medications, dietary changes, and lifestyle changes to achieve and maintain robust and lasting remission and to support the many ups and downs of living with this chronic condition. A diverse and well-rounded team of healthcare practitioners can help better address the diverse needs of IBD patients. Some of the most common healthcare professionals IBDers benefit from include:
- Primary Care Provider
- Gastroenterologist
- Registered Dietitian (RDN) or Nutritionist
- Integrative, Naturopathic, or Functional Medicine Practitioner
- Therapist, Psychologist, or Psychiatrist
- Life Coach
Many IBD patients with mild to moderate symptoms rely almost exclusively on their PCP for care. PCPs are typically the first stop for medical care in healthcare systems like that in the United States. PCPs are often the most familiar with day-to-day changes in a patient’s health status and can help monitor for the presence of new symptoms, extra-intestinal manifestations, and complications.
Gastroenterologists specialize in the gut and digestive health issues, with some specializing in IBD.62 Most IBDers will have established a relationship with a gastroenterologist during the diagnostic process. Maintaining a close and trusting relationship with a gastroenterologist is essential for strategizing and maintaining your primary approach to IBD treatment.
Nutritionists and RDNs have slightly different educational backgrounds and credentials. Nutritionists are not required by most states or countries to have extensive nutrition education or credentials, though many have completed training courses or certificate programs. Registered dietitians focus exclusively on nutrition and undergo extensive education and training including a master’s degree, a 1-year-long internship, and the board credentialing exam in the United States.63,64 Nutritionists and RDNs can be instrumental in developing a dietary strategy that is nutritionally adequate, enjoyable, and accessible for people with special dietary needs.
Integrative medicine specialists, naturopathic doctors, and functional medicine specialists often develop more holistic treatment approaches and may incorporate treatment strategies that reach beyond standard frontline medications.65 While naturopathic medicine alone is not a suitable replacement for primary care providers and gastroenterologists, their treatment approach may be able to complement and support your existing protocol. Always seek approval from your PCP or GI for new procedures.
Mental health specialists can be invaluable in learning to manage the stressors of living with IBD and all of the emotions that come with it. For most of us, IBD takes a serious toll on mental health and relationships.66 Taking care of your mental health and mindset can dramatically improve treatment outcomes.67–70
Many IBDers report that managing their conditions “feels like a full-time job,” and a life coach can help you find balance and promote accountability for all of your commitments and goals.71 This includes not only your IBD protocol but also other aspects of your life.
A well-rounded healthcare team can ensure that all of your needs are met. IBD is a multifaceted condition that requires a multidisciplinary approach. When establishing relationships with new healthcare providers, it is essential to find practitioners that make you feel heard and respected, are open to your input, and are willing to respect and consider your unique goals and needs. If you ever feel ignored, shamed, or uncomfortable with your healthcare provider, consider finding another practitioner who is a better fit for your needs.
Navigating Contradictory IBD Treatment Advice
One reality that most people with IBD face when navigating their healthcare is being confronted with conflicting advice and contradictory sources of information. Much of this is because our understanding of IBD treatments is evolving every single day. Researchers and healthcare providers are constantly expanding their knowledge of which medications are most effective when, how to incorporate dietary and lifestyle strategies that work best for different individuals, and more. Staying up-to-date with the latest developments on IBD treatments is essential to getting the best possible advice for IBD treatments. Additionally, avoiding one-sided sources of information and sources that are strictly “anti-medication” or “anti-natural approach” can help ensure information is unbiased and more accurate. While each IBDer is entitled to develop their own treatment goals and have their own opinions about which strategies they are interested in pursuing, it is important to understand there is evidence to support both medical treatment options and natural or holistic treatments for IBD. There is no one-size-fits-all treatment for IBD and any source claiming the contrary is misguiding their followers.
Monitoring Symptoms of IBD
The day-to-day symptoms experienced by most individuals with IBD are some of the clearest signs of how disease activity is doing. Many IBDers find that their frequency and consistency of bowel movements, abdominal pain and cramping, blood or mucus in the stool, and even stress can be very direct indicators of how their IBD is doing. In many cases, some symptoms may even serve as early warning signs of a coming flare. Monitoring symptoms of IBD in a journal or app, even in times of remission, can be a great way to keep a record of disease activity.72 Keeping track of symptoms of IBD can help monitor for signs of a coming flare and observe if changes to medications, diet, lifestyle, or stress have had a positive (or negative) impact on your IBD. Many IBDers find that it is hard to tune into their symptoms and notice immediate changes at first, but listening to your body and noticing subtle changes is a skill that can improve with time and practice. Over time, it is possible to uncover surprising patterns in symptoms that you never thought possible—one member of the IBDCoach program, for example, found that their eczema consistently got worse several weeks preceding an IBD flare. By tuning into this symptom, they were able to stop future flares from escalating by jumping into their flare protocol at the first sign of skin symptoms.
Monitoring Inflammatory Markers of IBD
Regular lab tests to assess inflammatory markers of IBD can be another extremely useful tool to monitor how well treatment interventions are working or to keep an eye out for signs of a flare during remission.73 One of the best inflammatory markers to monitor IBD activity is also used during the diagnosis of IBD: fecal calprotectin. Increasing levels of fecal calprotectin strongly correlate to increased inflammation in the GI tract and increased disease activity. Regular fecal calprotectin tests can help determine if inflammation is decreasing in response to treatment interventions or increasing as a result of a flare.74–76 Other inflammatory markers that some IBDers find helpful to monitor to help manage their IBD include C-reactive protein (CRP) and sedimentation rate, both of which can be measured with a blood test.73 In addition to monitoring laboratory markers of IBD, physicians may utilize additional screening tests or questionnaires as a part of their regular IBD monitoring protocol.77,78
Managing an IBD Flare
With inflammatory bowel disease, flares happen. Whether symptoms of IBD are increasing or rising calprotectin levels have hinted at an early warning sign of a flare, IBD flares require expedient and intentional treatment before the symptoms become debilitating. As we discussed above, many of the complications of IBD are heavily associated with prolonged duration of inflammation so it is best to not let flares get out of hand or go on for extended periods. While flares may often feel out of your control, being in tune with early warning signs and having a plan in place before a flare strikes can make a big difference in getting things under control as quickly as possible. You have a lifetime to refine your flare protocol, so it is okay if it isn’t perfect just yet.
Adapting Your IBD Protocol to Changes
If one thing is true about IBD, it is that IBD is unpredictable. Flares surprise us, our tried and true treatment plans may stop working someday, symptoms and sensitivities change, and triggers come and go. Monitoring symptoms of IBD and having a plan in place to tackle a flare is essential to managing IBD in the long term. A key part of both of these elements of IBD management is learning to adapt your IBD protocol and plan for changes. While it can be easy to find what works and stick to that plan religiously, nothing in IBD is ever set in stone. Here are a few key ways to be sure to adapt your protocol to changes over time:
- Experiment (thoughtfully) with your diet. Many IBDers find themselves on rigid and highly restricted diets. In fact, a majority of IBDers have dietary habits that are so restrictive that they show some signs of disordered eating or conditions like avoidant-restrictive food intake disorder (AFRID).79–82 While it can be hard to risk disturbing the peace to experiment with diet during periods of remission, it can be good for your physical and emotional health to introduce new foods into your diet when possible. At IBDCoach, we call these intentional dietary experimentations “Explorations.”
- Pay attention to extraintestinal manifestations (EIMS) of IBD. Many individuals with IBD experience EIMs, or symptoms of IBD that manifest outside of the GI tract, which we discuss in detail in Part One of This Blog Series.83–85 Severity of EIMs often mirrors IBD activity, so paying attention to these more subtle signs may be early indicators of flares and reminders to adjust your protocol to get back on track.
- Don’t get stuck in a black and white mindset toward natural treatments for IBD or medications for IBD. Natural treatments for IBD can be effective. Medications for IBD can be effective. For almost all IBDers, a combination of both is typically the most effective treatment for their IBD. If symptoms are creeping back or a flare has been particularly challenging, consider adjusting the balance between frontline treatment strategies like medications or complementary approaches like diet and lifestyle.
- Dial back on stressors. Stress plays a central role in inflammatory bowel disease.52 Sometimes doing less is more. Consider removing things from your plate and making more space for rest and recovery if you are struggling to get the upper hand on an IBD flare.
These are just some of the many ways you can continually adjust and fine-tune your IBD treatment plant. The perfect IBD protocol is fluid and adaptable to your current needs, goals, and level of disease activity. Pay attention to what changes have a positive impact and which ones do not. Most importantly, remember that there is always room for adjustment and improvement. Flares are not failures; instead, they are signs that it is time to make a change in your protocol and keep moving forward. If you remain flexible and ready to adapt to surprises, you will learn to more successfully and more quickly navigate the many ups and downs of living with IBD.
The Mental and Emotional Toll of Living with IBD
Inflammatory bowel disease is not just a gastrointestinal condition. The effects of living with a chronic, lifetime condition like IBD are far-reaching. IBD impacts all facets of life: social relationships, intimate relationships, family dynamics, career goals, educational opportunities, self-love, body image, and more. These are all more difficult to navigate when living with such a complicated, mysterious, and incurable condition. Many resources for IBD care leave out these facets of life with IBD. They assume that if the IBD is being effectively treated, all else is fine. This is simply not true. The physical symptoms of IBD are hard enough, but in many cases, the hidden side effects of IBD can be even more burdensome.
Hidden Toll of Living with IBD
Shying away from discussing the many hardships that people with IBD face outside of the doctor’s office hurts our ability to understand these facets of IBD and overcome them. While the ways in which IBD can impact day-to-day life are almost infinite, some of the most common hidden costs of living with IBD that we frequently see discussed in our communities are:
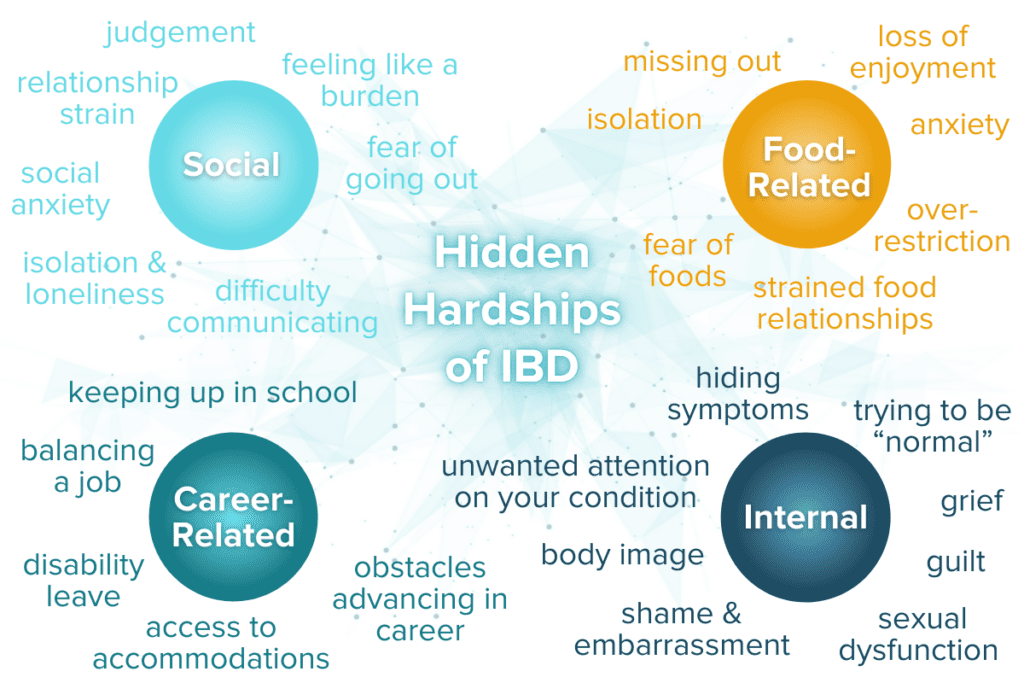
Time and time again, we’ve seen members of the IBD community discuss grappling with these hurdles, but this barely scratches the surface of the myriad ways IBD impacts life outside of the GI tract. Our social, intrapersonal, food-related, and professional lives are affected by IBD. These struggles, and many others that we have undoubtedly failed to cover, are linked to all facets of health and wellbeing. Acknowledging the ways that IBD impacts day-to-day life can help make the necessary space for healing, self-love and compassion.
Finding Support
One of the most invaluable parts of the IBDCoach program is a global community of IBDers that are available to support each other. Many of the hidden tolls of living with IBD are not obscure and isolated struggles: they are common battles that most of us contend with along this lifelong journey. Even in remission and with the most robust support systems in place, IBD can continue to take a hidden toll on patients. Finding understanding peers and support for the hidden struggles of IBD can be a life-changing step on the road to remission. Many support communities exist around the world including online groups, in-person events and therapists that specialize in grief and chronic health conditions. If you are feeling alone in your struggle with IBD, we see you and we have been there but know that you are not alone.
To learn more about how IBDCoach provides support to our community, schedule an Admissions Call today.
Support for IBD Caregivers
At IBDCoach, we know that inflammatory bowel disease is a family affair. The invisible nature of the condition makes it all the more challenging for family and friends to understand and support someone with IBD, and it isn’t intuitive to people on the outside just how many areas of day-to-day life are affected by this GI condition. IBD symptoms like frequency and urgency, dietary restriction, fatigue, and mental health distress can impact a person’s ability to participate in the workplace, enjoy social events, and attend to family responsibilities. These scenarios can all lead to misunderstandings between the IBDer and their family and community which can add stress to relationships.
In addition, members of an IBD patient’s support network who are highly involved in helping manage their loved one’s IBD like parents, spouses, children, and close friends can be at risk of caregiver burnout due to the extra responsibilities of supporting their loved ones. Some important points for IBD caregivers to keep in mind to help support themselves are:
- Caregivers need to take care of themselves too: you can’t pour from an empty cup. Set aside time for self-care and space to address personal needs or to enjoy a hobby or alone time.
- Good communication work and respect for boundaries (self and others) are all the more important to maintain a productive relationship between IBDer and caregiver
- A caregiving relationship can feel a little one-sided and narrowly focused, so maintain an aspect of the relationship that isn’t focused on the IBD (spend time talking about non-IBD things)
- Caregivers can educate themselves and find a community of peers to direct questions to and receive support in ways that don’t place responsibility on the IBDer
Very few resources exist to support IBD caregivers and the loved ones of people with IBD on their journey. IBD touches the lives of our loved ones in unexpected ways and the need for additional support is an important part of the IBD care process. At IBDCoach, we provide a network of support resources for both our members with IBD and those closest to them. Healing doesn’t happen in isolation.
To learn more about our support resources for families, schedule an Admissions Call today.
Remission is a Way of Life
In the words of our founder, Andrew Kornfeld: Remission is not a destination. Remission is a way of life.
For most IBDers, the GI symptoms of Crohn’s disease, ulcerative colitis, or microscopic colitis are only just the beginning. Inflammatory bowel disease, with all of its ups and downs, touches all aspects of life. Our relationships with ourselves, with friends and family, with food, and with our professional goals are intimately connected to IBD as part of a delicate and expansive system. This complicated network is exactly why remission is a way of life, not just a singular goal or destination. In the thick of a flare, remission can feel like a far-off fantasy or an impossible alternate reality. But in the depths of the valley, it is hard to see the horizon. We know remission is possible for every single IBDer out there. IBDCoach’s mission is to help every last IBDer get there. Remission is a way of life—are you ready to come on this journey with us and make it yours?
- Alatab S, Sepanlou SG, Ikuta K, et al. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5(1):17-30. doi:10.1016/S2468-1253(19)30333-4
- Kaplan GG. The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol. 2015;12(12):720-727. doi:10.1038/nrgastro.2015.150
- Kaplan GG, Windsor JW. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2021;18(1):56-66. doi:10.1038/s41575-020-00360-x
- Boland K, Nguyen GC. Microscopic Colitis: A Review of Collagenous and Lymphocytic Colitis. Gastroenterol Hepatol. 2017;13(11):671-677.
- Pardi DS. Diagnosis and Management of Microscopic Colitis. Am J Gastroenterol. 2017;112(1):78-85. doi:10.1038/ajg.2016.477
- Weimers P, Ankersen DV, Lophaven S, et al. Incidence and Prevalence of Microscopic Colitis Between 2001 and 2016: A Danish Nationwide Cohort Study. J Crohns Colitis. 2020;14(12):1717-1723. doi:10.1093/ecco-jcc/jjaa108
- What is IBD? Crohn’s & Colitis Foundation. Accessed November 5, 2021. https://www.crohnscolitisfoundation.org/what-is-ibd
- CDC -What is inflammatory bowel disease (IBD)? – Inflammatory Bowel Disease – Division of Population Health. Published May 11, 2020. Accessed November 5, 2021. https://www.cdc.gov/ibd/what-is-IBD.htm
- Microscopic colitis – Symptoms and causes. Mayo Clinic. Accessed March 21, 2022. https://www.mayoclinic.org/diseases-conditions/microscopic-colitis/symptoms-causes/syc-20351478
- de Mattos BRR, Garcia MPG, Nogueira JB, et al. Inflammatory Bowel Disease: An Overview of Immune Mechanisms and Biological Treatments. Mediators Inflamm. 2015;2015:493012. doi:10.1155/2015/493012
- Ramos GP, Papadakis KA. Mechanisms of Disease: Inflammatory Bowel Diseases. Mayo Clin Proc. 2019;94(1):155-165. doi:10.1016/j.mayocp.2018.09.013
- Cho JH. The genetics and immunopathogenesis of inflammatory bowel disease. Nat Rev Immunol. 2008;8(6):458-466. doi:10.1038/nri2340
- Cleynen I, Boucher G, Jostins L, et al. Inherited determinants of Crohn’s disease and ulcerative colitis phenotypes: a genetic association study. The Lancet. 2016;387(10014):156-167. doi:10.1016/S0140-6736(15)00465-1
- Loddo I, Romano C. Inflammatory Bowel Disease: Genetics, Epigenetics, and Pathogenesis. Front Immunol. 2015;6:551. doi:10.3389/fimmu.2015.00551
- Andersen V, Olsen A, Carbonnel F, Tjønneland A, Vogel U. Diet and risk of inflammatory bowel disease. Dig Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver. 2012;44(3):185-194. doi:10.1016/j.dld.2011.10.001
- Chiba M, Nakane K, Komatsu M. Westernized Diet is the Most Ubiquitous Environmental Factor in Inflammatory Bowel Disease. Perm J. 2019;23:18-107. doi:10.7812/TPP/18-107
- Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. 2015;12(4):205-217. doi:10.1038/nrgastro.2015.34
- Carreras-Torres R, Ibáñez-Sanz G, Obón-Santacana M, Duell EJ, Moreno V. Identifying environmental risk factors for inflammatory bowel diseases: a Mendelian randomization study. Sci Rep. 2020;10(1):19273. doi:10.1038/s41598-020-76361-2
- Khalili H, Granath F, Smedby KE, et al. Association Between Long-term Oral Contraceptive Use and Risk of Crohn’s Disease Complications in a Nationwide Study. Gastroenterology. 2016;150(7):1561-1567.e1. doi:10.1053/j.gastro.2016.02.041
- Armstrong H, Mander I, Zhang Z, Armstrong D, Wine E. Not All Fibers Are Born Equal; Variable Response to Dietary Fiber Subtypes in IBD. Front Pediatr. 2021;8. doi:10.3389/fped.2020.620189
- Basso PJ, Câmara NOS, Sales-Campos H. Microbial-Based Therapies in the Treatment of Inflammatory Bowel Disease – An Overview of Human Studies. Front Pharmacol. 2019;9:1571. doi:10.3389/fphar.2018.01571
- Cai Z, Wang S, Li J. Treatment of Inflammatory Bowel Disease: A Comprehensive Review. Front Med. 2021;8. Accessed March 21, 2022. https://www.frontiersin.org/article/10.3389/fmed.2021.765474
- González-Gallego J, García-Mediavilla MV, Sánchez-Campos S, Tuñón MJ. Anti-inflammatory, Immunomodulatory, and Prebiotic Properties of Dietary Flavonoids. In: Polyphenols: Prevention and Treatment of Human Disease. Elsevier; 2018:327-345. doi:10.1016/B978-0-12-813008-7.00028-X
- Baliga MS, Joseph N, Venkataranganna MV, Saxena A, Ponemone V, Fayad R. Curcumin, an active component of turmeric in the prevention and treatment of ulcerative colitis: preclinical and clinical observations. Food Funct. 2012;3(11):1109-1117. doi:10.1039/c2fo30097d
- Househam AM, Peterson CT, Mills PJ, Chopra D. The Effects of Stress and Meditation on the Immune System, Human Microbiota, and Epigenetics. Adv Mind Body Med. 2017;31(4):10-25.
- Conlon M, Bird A. The Impact of Diet and Lifestyle on Gut Microbiota and Human Health. Nutrients. 2014;7(1):17-44. doi:10.3390/nu7010017
- Flanagan TW, Nichols CD. Psychedelics as anti-inflammatory agents. Int Rev Psychiatry. 2018;30(4):363-375. doi:10.1080/09540261.2018.1481827
- Aleksandrova LR, Phillips AG. Neuroplasticity as a convergent mechanism of ketamine and classical psychedelics. Trends Pharmacol Sci. 2021;42(11):929-942. doi:10.1016/j.tips.2021.08.003
- de Vos CMH, Mason NL, Kuypers KPC. Psychedelics and Neuroplasticity: A Systematic Review Unraveling the Biological Underpinnings of Psychedelics. Front Psychiatry. 2021;12. Accessed February 27, 2022. https://www.frontiersin.org/article/10.3389/fpsyt.2021.724606
- Farrell D, McCarthy G, Savage E. Self-reported Symptom Burden in Individuals with Inflammatory Bowel Disease. J Crohns Colitis. 2016;10(3):315-322. doi:10.1093/ecco-jcc/jjv218
- Ballou S, Hirsch W, Singh P, et al. Emergency Department Utilization for Inflammatory Bowel Disease in the United States from 2006–2014. Aliment Pharmacol Ther. 2018;47(7):913-921. doi:10.1111/apt.14551
- Signs and Symptoms of Crohn’s Disease. Crohn’s & Colitis Foundation. Accessed April 4, 2022. https://www.crohnscolitisfoundation.org/what-is-crohns-disease/symptoms
- Chang CW, Wong JM, Tung CC, Shih IL, Wang HY, Wei SC. Intestinal Stricture in Crohn’s Disease. Intest Res. 2015;13(1):19-26. doi:10.5217/ir.2015.13.1.19
- Schwartz DA, Tagarro I, Carmen Díez M, Sandborn WJ. Prevalence of Fistulizing Crohn’s Disease in the United States: Estimate From a Systematic Literature Review Attempt and Population-Based Database Analysis. Inflamm Bowel Dis. 2019;25(11):1773-1779. doi:10.1093/ibd/izz056
- Skomorochow E, Pico J. Toxic Megacolon. In: StatPearls. StatPearls Publishing; 2022. Accessed April 4, 2022. http://www.ncbi.nlm.nih.gov/books/NBK547679/
- Clarke WT, Feuerstein JD. Colorectal cancer surveillance in inflammatory bowel disease: Practice guidelines and recent developments. World J Gastroenterol. 2019;25(30):4148-4157. doi:10.3748/wjg.v25.i30.4148
- Lakatos PL, Lakatos L. Risk for colorectal cancer in ulcerative colitis: Changes, causes and management strategies. World J Gastroenterol WJG. 2008;14(25):3937-3947. doi:10.3748/wjg.14.3937
- Castaño-Milla C, Chaparro M, Gisbert JP. Systematic review with meta-analysis: the declining risk of colorectal cancer in ulcerative colitis. Aliment Pharmacol Ther. 2014;39(7):645-659. doi:10.1111/apt.12651
- Jess T, Simonsen J, Jørgensen KT, Pedersen BV, Nielsen NM, Frisch M. Decreasing Risk of Colorectal Cancer in Patients With Inflammatory Bowel Disease Over 30 Years. Gastroenterology. 2012;143(2):375-381.e1. doi:10.1053/j.gastro.2012.04.016
- Bähler C, Schoepfer AM, Vavricka SR, Brüngger B, Reich O. Chronic comorbidities associated with inflammatory bowel disease: prevalence and impact on healthcare costs in Switzerland. Eur J Gastroenterol Hepatol. 2017;29(8):916-925. doi:10.1097/MEG.0000000000000891
- Orchard TR. Management of Arthritis in Patients with Inflammatory Bowel Disease. Gastroenterol Hepatol. 2012;8(5):327-329.
- Chao YS, Loshak H. Biologics versus Immunomodulators for the Treatment of Ulcerative Colitis: A Review of Comparative Clinical Effectiveness and Cost-Effectiveness. Canadian Agency for Drugs and Technologies in Health; 2019. Accessed April 4, 2022. http://www.ncbi.nlm.nih.gov/books/NBK549363/
- Askar S, Sakr MA, Alaty WHA, et al. The psychological impact of inflammatory bowel disease as regards anxiety and depression: a single-center study. Middle East Curr Psychiatry. 2021;28(1):73. doi:10.1186/s43045-021-00154-0
- Marrie RA, Walker JR, Graff LA, et al. Performance of administrative case definitions for depression and anxiety in inflammatory bowel disease. J Psychosom Res. 2016;89:107-113. doi:10.1016/j.jpsychores.2016.08.014
- Mikocka-Walus A, Pittet V, Rossel JB, et al. Symptoms of Depression and Anxiety Are Independently Associated With Clinical Recurrence of Inflammatory Bowel Disease. Clin Gastroenterol Hepatol. 2016;14(6):829-835.e1. doi:10.1016/j.cgh.2015.12.045
- Brustolim D, Ribeiro-dos-Santos R, Kast RE, Altschuler EL, Soares MBP. A new chapter opens in anti-inflammatory treatments: the antidepressant bupropion lowers production of tumor necrosis factor-alpha and interferon-gamma in mice. Int Immunopharmacol. 2006;6(6):903-907. doi:10.1016/j.intimp.2005.12.007
- Neuendorf R, Harding A, Stello N, Hanes D, Wahbeh H. Depression and anxiety in patients with Inflammatory Bowel Disease: A systematic review. J Psychosom Res. 2016;87:70-80. doi:10.1016/j.jpsychores.2016.06.001
- Taft TH, Quinton S, Jedel S, Simons M, Mutlu EA, Hanauer SB. Posttraumatic Stress in Patients With Inflammatory Bowel Disease: Prevalence and Relationships to Patient-Reported Outcomes. Inflamm Bowel Dis. Published online June 17, 2021:izab152. doi:10.1093/ibd/izab152
- Cámara RJA, Gander ML, Begré S, Känel R von, Group SIBDCS. Post-traumatic stress in Crohn’s disease and its association with disease activity. Frontline Gastroenterol. 2011;2(1):2-9. doi:10.1136/fg.2010.002733
- Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB. Cumulative Childhood Stress and Autoimmune Diseases in Adults. Psychosom Med. 2009;71(2):243-250. doi:10.1097/PSY.0b013e3181907888
- Glynn H, Möller SP, Wilding H, Apputhurai P, Moore G, Knowles SR. Prevalence and Impact of Post-traumatic Stress Disorder in Gastrointestinal Conditions: A Systematic Review. Dig Dis Sci. 2021;66(12):4109-4119. doi:10.1007/s10620-020-06798-y
- Sun Y, Li L, Xie R, Wang B, Jiang K, Cao H. Stress Triggers Flare of Inflammatory Bowel Disease in Children and Adults. Front Pediatr. 2019;7:432. doi:10.3389/fped.2019.00432
- Sebastian S, Neilaj S. Practical guidance for the management of inflammatory bowel disease in patients with cancer. Which treatment? Ther Adv Gastroenterol. 2019;12:1756284818817293. doi:10.1177/1756284818817293
- Mason M, Siegel CA. Do inflammatory bowel disease therapies cause cancer? Inflamm Bowel Dis. 2013;19(6):1306-1321. doi:10.1097/MIB.0b013e3182807618
- Pinto-Sanchez MI, Seiler CL, Santesso N, et al. Association Between Inflammatory Bowel Diseases and Celiac Disease: A Systematic Review and Meta-Analysis. Gastroenterology. 2020;159(3):884-903.e31. doi:10.1053/j.gastro.2020.05.016
- Lemaitre M, Kirchgesner J, Rudnichi A, et al. Association Between Use of Thiopurines or Tumor Necrosis Factor Antagonists Alone or in Combination and Risk of Lymphoma in Patients With Inflammatory Bowel Disease. JAMA. 2017;318(17):1679-1686. doi:10.1001/jama.2017.16071
- Dahmus J, Rosario M, Clarke K. <p>Risk of Lymphoma Associated with Anti-TNF Therapy in Patients with Inflammatory Bowel Disease: Implications for Therapy</p>. Clin Exp Gastroenterol. 2020;13:339-350. doi:10.2147/CEG.S237646
- Anti-TNF therapy could lower colorectal cancer risk for IBD patients. Crohn’s & Colitis Foundation. Accessed April 4, 2022. https://www.crohnscolitisfoundation.org/blog/anti-tnf-therapy-could-lower-colorectal-cancer-risk-ibd-patients
- Lucafò M, Curci D, Franzin M, Decorti G, Stocco G. Inflammatory Bowel Disease and Risk of Colorectal Cancer: An Overview From Pathophysiology to Pharmacological Prevention. Front Pharmacol. 2021;12. Accessed April 4, 2022. https://www.frontiersin.org/article/10.3389/fphar.2021.772101
- Stidham RW, Higgins PDR. Colorectal Cancer in Inflammatory Bowel Disease. Clin Colon Rectal Surg. 2018;31(3):168-178. doi:10.1055/s-0037-1602237
- Algaba A, Guerra I, Marin-Jimenez I, et al. Incidence, Management, and Course of Cancer in Patients with Inflammatory Bowel Disease. J Crohns Colitis. 2015;9(4):326-333. doi:10.1093/ecco-jcc/jjv032
- What is a Gastroenterologist? American College of Gastroenterology. Accessed April 4, 2022. https://gi.org/patients/gi-health-and-disease/what-is-a-gastroenterologist/
- What is a Registered Dietitian Nutritionist. Accessed April 4, 2022. https://www.eatrightpro.org/about-us/what-is-an-rdn-and-dtr/what-is-a-registered-dietitian-nutritionist
- 2024 Graduate Degree Requirement: Registration Examination Eligibility. Accessed April 4, 2022. https://www.eatrightpro.org/acend/program-directors/program-directors-faqs/2024-graduate-degree-requirement
- Complementary Medicine. Crohn’s & Colitis Foundation. Accessed April 4, 2022. https://www.crohnscolitisfoundation.org/ibd/complementary-medicine
- Gamwell KL, Roberts CM, Espeleta HC, et al. Perceived stigma, illness uncertainty, and depressive symptoms in youth with inflammatory bowel disease: The moderating effect of mindfulness. Psychol Health Med. 2020;25(9):1037-1048. doi:10.1080/13548506.2020.1714062
- Sarrasin JB, Nenciovici L, Foisy LMB, Allaire-Duquette G, Riopel M, Masson S. Effects of teaching the concept of neuroplasticity to induce a growth mindset on motivation, achievement, and brain activity: A meta-analysis. Trends Neurosci Educ. 2018;12:22-31. doi:10.1016/j.tine.2018.07.003
- Ewais T, Begun J, Kenny M, et al. Mindfulness based cognitive therapy for youth with inflammatory bowel disease and depression – Findings from a pilot randomised controlled trial. J Psychosom Res. 2021;149:110594. doi:10.1016/j.jpsychores.2021.110594
- Jedel S, Hoffman A, Merriman P, et al. A Randomized Controlled Trial of Mindfulness Based Stress Reduction to Prevent Flare-up in Patients with Inactive Ulcerative Colitis. Digestion. 2014;89(2):142-155. doi:10.1159/000356316
- González-Moret R, Cebolla A, Cortés X, et al. The effect of a mindfulness-based therapy on different biomarkers among patients with inflammatory bowel disease: a randomised controlled trial. Sci Rep. 2020;10(1):6071. doi:10.1038/s41598-020-63168-4
- What Does a Life Coach Do? Verywell Mind. Accessed April 4, 2022. https://www.verywellmind.com/what-is-a-life-coach-4129726
- How to Track Your Crohn’s Symptoms. EverydayHealth.com. Accessed April 4, 2022. https://www.everydayhealth.com/hs/crohns-disease-treatment-management/track-crohns-symptoms/
- Sands BE. Biomarkers of Inflammation in Inflammatory Bowel Disease. Gastroenterology. 2015;149(5):1275-1285.e2. doi:10.1053/j.gastro.2015.07.003
- Bjarnason I. The Use of Fecal Calprotectin in Inflammatory Bowel Disease. Gastroenterol Hepatol. 2017;13(1):53-56.
- Pathirana WGW, Chubb SP, Gillett MJ, Vasikaran SD. Faecal Calprotectin. Clin Biochem Rev. 2018;39(3):77-90.
- Khaki-Khatibi F, Qujeq D, Kashifard M, Moein S, Maniati M, Vaghari-Tabari M. Calprotectin in inflammatory bowel disease. Clin Chim Acta Int J Clin Chem. 2020;510:556-565. doi:10.1016/j.cca.2020.08.025
- Gonczi L, Bessissow T, Lakatos PL. Disease monitoring strategies in inflammatory bowel diseases: What do we mean by “tight control”? World J Gastroenterol. 2019;25(41):6172-6189. doi:10.3748/wjg.v25.i41.6172
- Plevris N, Lees CW. Disease Monitoring in Inflammatory Bowel Disease: Evolving Principles and Possibilities. Gastroenterology. 2022;0(0). doi:10.1053/j.gastro.2022.01.024
- Marsh A, Kinneally J, Robertson T, Lord A, Young A, Radford –Smith G. Food avoidance in outpatients with Inflammatory Bowel Disease – Who, what and why. Clin Nutr ESPEN. 2019;31:10-16. doi:10.1016/j.clnesp.2019.03.018
- Yelencich E, Truong E, Widaman AM, et al. Avoidant Restrictive Food Intake Disorder Prevalent Among Patients With Inflammatory Bowel Disease. Clin Gastroenterol Hepatol. 2021;0(0). doi:10.1016/j.cgh.2021.08.009
- Day AS, Yao CK, Costello SP, Andrews JM, Bryant RV. Food‐related quality of life in adults with inflammatory bowel disease is associated with restrictive eating behaviour, disease activity and surgery: A prospective multicentre observational study. J Hum Nutr Diet. 2022;35(1):234-244. doi:10.1111/jhn.12920
- Larussa T, Suraci E, Marasco R, Imeneo M, Abenavoli L, Luzza F. Self-Prescribed Dietary Restrictions are Common in Inflammatory Bowel Disease Patients and Are Associated with Low Bone Mineralization. Medicina (Mex). 2019;55(8):507. doi:10.3390/medicina55080507
- Levine JS, Burakoff R. Extraintestinal Manifestations of Inflammatory Bowel Disease. Gastroenterol Hepatol. 2011;7(4):235-241.
- Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal Manifestations of Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21(8):1982-1992. doi:10.1097/MIB.0000000000000392
- Extraintestinal Complications of IBD. Crohn’s & Colitis Foundation. Accessed March 21, 2022. https://www.crohnscolitisfoundation.org/what-is-ibd/extraintestinal-complications-ibd





