What Causes IBD?
To date, no one has a definitive understanding of what causes or worsens Inflammatory Bowel Diseases like Crohn’s disease, ulcerative colitis, or microscopic colitis. However, it is understood that a range of genetic and environmental factors can contribute to developing IBD. Studies of genetically identical twins show very low rates of IBD presenting in both twins, though the rates are slightly higher than comparisons of two more distantly related individuals.1 In fact, over 200 genes have been identified as playing a role in IBD risk, but no single gene stands out as a consistently causal factor. A complex interplay of genes and environmental factors must coalesce in the “perfect storm”. The immune system, the microbiome, the nervous system, diet, stress, medications, and even mitochondrial DNA may all play a role in IBD. But one factor common in half the population that doesn’t get enough discussion is the use of hormonal contraceptives.
Learn More About Symptoms, Causes, and Risk Factors for IBD
The Evidence Linking Oral Contraceptives and IBD
There is no definitive cause of IBD, but a strong body of evidence indicates that oral contraceptives increase the risk of developing IBD more than almost any other environmental factor. In a 2016 review article, inflammatory bowel disease expert Dr. Hamed Khalili, MD, MPH of Harvard Medical School stated: “Beyond smoking, perhaps the most consistent environmental risk factor for Crohn’s disease is the use of oral contraceptives.”2 (Note: Tobacco use and smoking are well-accepted environmental risk factors for developing Crohn’s disease, but it also appears that smoking combined with oral contraceptives magnifies this risk).
What exactly have the studies consistently linking oral contraceptives to IBD shown? A meta-analysis from 2008 of 14 studies indicated a nearly 50% increase in the risk of developing Crohn’s disease among individuals using oral contraceptives.3,4 For ulcerative colitis, the data was less definitive but there may have also been a less significant link.5 In large prospective studies with over 200,000 women and females, researchers uncovered an increased risk of developing CD but not UC among participants using oral contraceptives.6,7 Most recently, a 2017 meta-analysis of 20 studies confirmed the results and found that among individuals taking oral contraceptives, there was a 24% increased risk for developing CD and a 30% increased risk for UC.6 A 2016 study in Sweden examining 4036 female CD patients demonstrated an increased probability of surgery among people taking oral contraceptives – especially in those who are on combination type.8 The evidence behind oral contraceptives seems clear: oral contraceptives may increase the risk of developing IBD in susceptible individuals. Do other forms of contraception carry the same risk?
Other Hormonal Contraceptives and IBD Risk
Unfortunately, there exists a major gap in the research regarding the use of other forms of hormonal contraceptives such as shots, implants and intrauterine devices (IUDs). Oral contraceptives may pose the greatest risk because they must interact directly with the gastrointestinal lining to be absorbed instead of acting locally in the uterus or in circulation such as an arm implant. In general, oral contraceptive pills are considered to release higher doses of hormones than other forms of birth control. If the hormones are a driving force behind the increased IBD, there is potential that other forms of oral contraceptives may have a lesser impact on IBD risk, though this has not been formally investigated.
Hormone Therapies and IBD Risk
The idea that hormonal birth control may increase IBD risk also raises the question of whether hormone replacement therapies may have a similar effect. Unfortunately, there is yet again a major gap in the scientific literature regarding people taking hormone replacement therapies and their risk of developing IBD. For individuals that this may apply to, it can be useful to consider the mechanisms by which hormones may impact IBD risk and pathogenesis to try to gain a deeper understanding of their situation. With that being said–can hormonal contraceptives or therapies impact IBD severity and outcomes?
Hormonal Contraceptives and IBD Severity
Evidence consistently demonstrates that the risk of developing IBD is increased in susceptible individuals that are taking oral contraceptives, so are people that already have IBD at risk of experiencing worse symptoms or disease activity if they take oral or hormonal contraceptives?
One study showed that more than half of the respondents to a survey regarding contraceptive use in people with IBD indicated that they use some form of hormonal contraception.9 Interestingly, this includes 17% using a “highly effective” hormonal contraceptive such as an IUD and 44% using a “moderately effective” hormonal contraceptive, which would likely include oral contraceptives. Another 19% use barrier methods. 23% of respondents reported that they do not use any form of contraception.
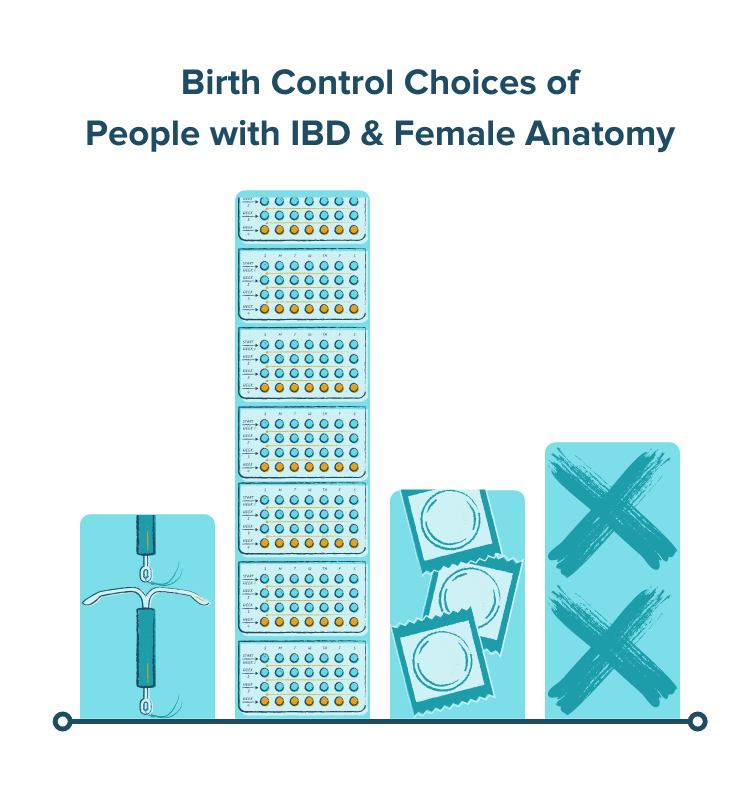
Aside from the study discussed above that indicates that oral contraceptive use may increase the risk of surgery in IBD, there are no formal and controlled studies investigating whether or not contraceptive use impacts IBD symptom severity. Surveys suggest that some people with IBD taking hormonal contraceptives actually report decreased symptoms such as cramping and gastrointestinal discomfort. This may be because many forms of hormonal contraception decrease cramping and menstrual blood production. The increased percentage of people reporting no contraceptive use, however, is interesting to ponder. Do more people with IBD opt-out of contraception use because of the risk factors? The mechanisms of action behind how hormonal contraceptives function may provide a few clues as to how they impact IBD pathogenesis.
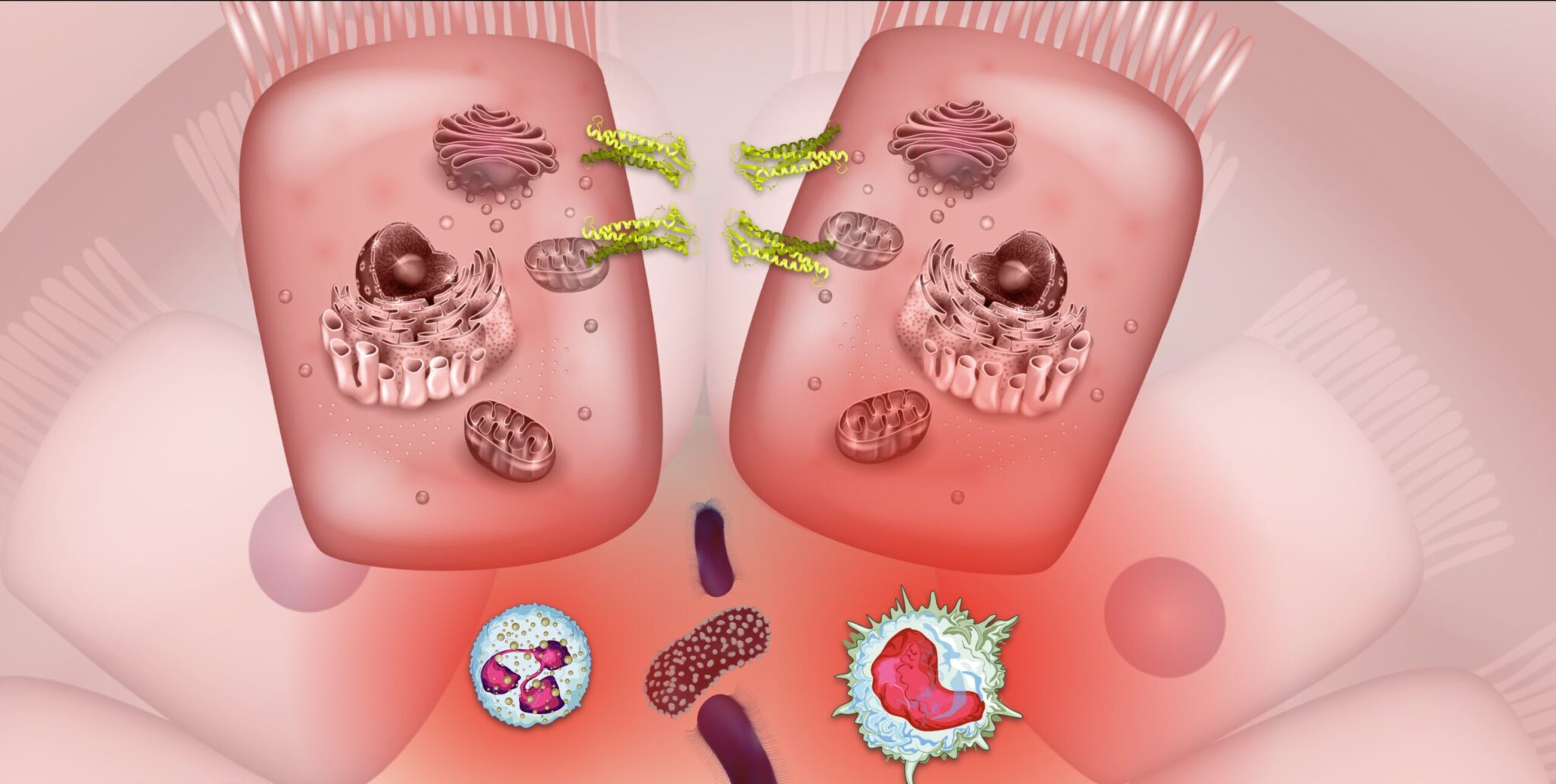
Mechanisms Linking Contraceptives to IBD Risk
Of all the hormones discussed in the context of contraceptives and IBD, it seems that the relationship between estrogen-containing contraceptives and IBD (primarily in Crohn’s disease) is strongest in regards to either disease development or likelihood of unfavorable outcomes (like surgery). Interestingly, progesterone-only contraceptives may not pose this risk and may even contribute to ameliorations in symptoms in women with CD.8,10
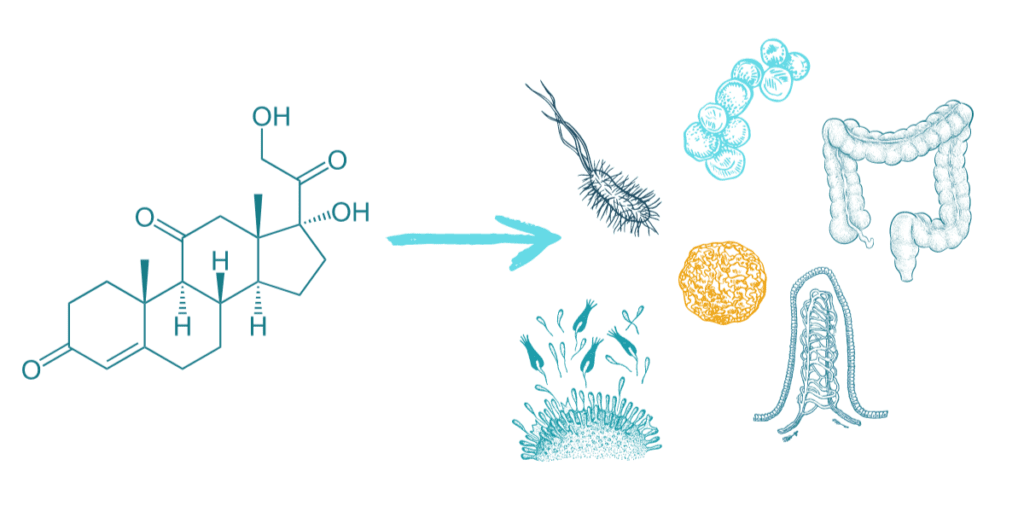
From a mechanistic standpoint, there may be several reasons why oral contraceptives magnify risk or worsen outcomes in IBD. Estrogen may modulate the mucosal immune system’s response, membrane permeability, and even the human microbiome’s composition among other mechanisms.2
Key Takeaways on Hormones, Birth Control, and IBD
In summary, there seems to be a growing body of evidence suggesting that oral contraceptives may play a role in IBD. The scientific evidence seems to be strongest in drawing correlations between the risk of developing Crohn’s disease with moderate evidence regarding the risk of developing ulcerative colitis in people taking oral contraceptives. Most experts also agree that the evidence is less strong and substantially more research is needed to understand how hormonal contraceptives impact disease severity and activity. Additionally, there is very little evidence regarding other forms of hormonal birth control and hormone replacement therapies.
Something important to remember in regards to this discussion is that there is no perfect solution to the problem at hand and every individual must gather as much evidence as possible to make the best decisions for their unique situation. Just because there is some risk between oral contraceptive use and developing inflammatory bowel disease does NOT mean that every person taking hormonal contraceptives will develop IBD. IBD requires a perfect storm of myriad factors to develop, and oral contraceptives are just one small piece of that storm. Additionally, for many people, there are great risks that go along with opting out of contraceptives or hormone therapies as well. For some, contraception is a necessary evil. For others, hormone therapies are life-saving.
We hope this post inspires you to dive deeper into understanding your perfect storm and what risk factors may be impacting your journey. With inflammatory bowel disease, knowledge is power and we hope to empower you to have better discussions with your healthcare team and make more individualized decisions for your IBD remission journey. As always, remember to never make changes to your healthcare protocol without first consulting with your doctor.
Interested in having more support on your IBD journey to help understand your perfect storm of risk factors? IBDCoach can help. Attend our FREE Microcourse: The Foundations of Remission and learn more about the IBD perfect storm and how you can harness the power of knowledge to develop your Remission Master Plan.
- Gordon H, Trier Moller F, Andersen V, Harbord M. Heritability in inflammatory bowel disease: from the first twin study to genome-wide association studies. Inflamm Bowel Dis. 2015;21(6):1428-1434. doi:10.1097/MIB.0000000000000393
- Khalili H. Risk of Inflammatory Bowel Disease with Oral Contraceptives and Menopausal Hormone Therapy: Current Evidence and Future Directions. Drug Saf. 2016;39(3):193-197. doi:10.1007/s40264-015-0372-y
- Timmer* A, Lloyd R. Sutherland* ‡, Martin§ F. Oral contraceptive use and smoking are risk factors for relapse in Crohn’s disease. Gastroenterology. 1998;114(6):1143-1150. doi:10.1016/S0016-5085(98)70419-6
- Logan RFA. Smoking, use of oral contraceptives, and medical induction of remission were risk factors for relapse in Crohn’s disease. Gut. 1999;44(3):311-312. doi:10.1136/gut.44.3.311
- Cornish JA, Tan E, Simillis C, Clark SK, Teare J, Tekkis PP. The risk of oral contraceptives in the etiology of inflammatory bowel disease: a meta-analysis. Am J Gastroenterol. 2008;103(9):2394-2400. doi:10.1111/j.1572-0241.2008.02064.x
- Ortizo R, Lee SY, Nguyen ET, Jamal MM, Bechtold MM, Nguyen DL. Exposure to oral contraceptives increases the risk for development of inflammatory bowel disease: a meta-analysis of case-controlled and cohort studies. Eur J Gastroenterol Hepatol. 2017;29(9):1064-1070. doi:10.1097/MEG.0000000000000915
- Khalili H, Higuchi LM, Ananthakrishnan AN, et al. Oral contraceptives, reproductive factors and risk of inflammatory bowel disease. Gut. 2013;62(8):1153-1159. doi:10.1136/gutjnl-2012-302362
- Khalili H, Granath F, Smedby KE, et al. Association Between Long-term Oral Contraceptive Use and Risk of Crohn’s Disease Complications in a Nationwide Study. Gastroenterology. 2016;150(7):1561-1567.e1. doi:10.1053/j.gastro.2016.02.041
- Gawron LM, Gawron AJ, Kasper A, Hammond C, Keefer L. Contraceptive Method Selection by Women with Inflammatory Bowel Diseases: A Cross-sectional Survey. Contraception. 2014;89(5):419-425. doi:10.1016/j.contraception.2013.12.01610.
- Long MD, Hutfless S. Shifting Away From Estrogen-Containing Oral Contraceptives in Crohn’s Disease. Gastroenterology. 2016;150(7):1518-1520. doi:10.1053/j.gastro.2016.04.032